The Importance Of Spare Capacity – Why Your Spine Needs A Safety Margin
What if your back pain isn’t just from one bad movement — but from constantly living on the edge of your spine’s limits? This is

Achilles tendinopathy is a condition that affects the Achilles tendon, which is the tendon connecting the calf muscle to the heel bone.
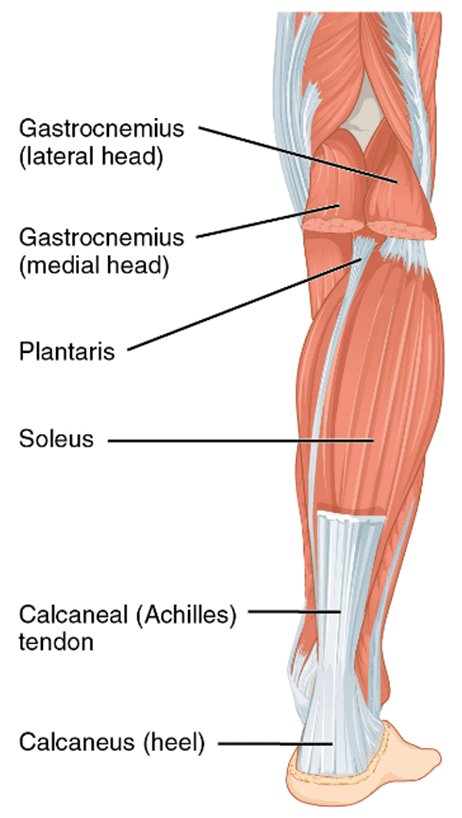
The Achilles tendon is the strongest and biggest tendon in our body and has the ability to resist large tensile forces. It originates from a distal joining of the gastrocnemius and soleus muscle and inserts at the bottom of the calcaneus.
The blood supply throughout the tendon is poor due to the small number of blood vessels that exist, especially in the region just above the calcaneus. This poor blood supply can result in a slower healing rate after injury or trauma.
The Achilles tendon is responsible for helping us walk, run, jump, and perform other physical activities. When running, the Achilles tendon experiences a force approximately 6-8 times of a person’s body weight every step. Due to this repetitive overload, the Achilles tendon is highly vulnerable to overuse injuries, such as Achilles tendinopathy.
Achilles tendinopathy is caused by repetitive stress to the tendon, which can result in changes of the tissue in the Achilles or sometimes small tears. The most common cause of the condition is overuse, particularly in athletes who engage in high-impact sports such as running. However, it can also occur in individuals who have been inactive for a long period of time and then suddenly increase their physical activity. When it becomes painful and inflamed, it can greatly affect an individual’s daily activities.
The causes of Achilles tendinopathy are complex and multifactorial, meaning the development of Achilles tendinopathy is often a result of multiple factors, and individual risk factors may interact with one another to contribute to the development of the condition. However, some commonly identified causes include:
Identifying and addressing these risk factors is an important part of managing and preventing Achilles tendinopathy.
Some of the common signs and symptoms of Achilles tendinopathy include:
The goal of Achilles tendinopathy treatment is to improve the ability of the tendon and associated muscles to work and manage load, which is known as the energy storage capacity. This allows the tendon to act like a ‘spring’ in storing and then releasing energy. The three key exercises for Achilles tendinopathy are:
Isometric tendon loading has pain-relieving effects, while also maintaining some baseline strength.
Depending on the symptoms and tendon irritability, Achilles tendon holds can either be performed double leg or single leg and can either be held mid or end of the range.
The goal of isotonic loading is to develop strength in the tendon and the surrounding muscles. In Achilles tendinopathy, the strength of the soleus and gastrocnemius muscles plays a major role.
These exercises are often commenced once the patient’s pain level and the tendon’s irritability reduces.
Isotonic seated calf raises can be performed with a gradual increase in loading. Each repetition should take 3-6 seconds to develop tension in the tendon.
Isotonic standing calf raises should be performed at the mid-range of the muscle’s movement. This ensures the tendon is not compressed, which can occur at the end of the range when exercising with heavier loads.
These exercises help the tendon to regain its capacity to absorb and then release energy via the stretch-shortening cycle.
These exercises are crucial to rehabilitation and can be commenced when the patient is progressing well with isotonic calf raises, has very mild tenderness when the Achilles tendon is touched, and has been able to tolerate light running without a flare-up in symptoms.
Plyometric exercises include:
o Double-leg hop
o Single leg hop
o Single leg step hops
o Hopscotch with activation band
Along with soft tissue occupational therapy, other treatment options include:
Load Management: Reducing the amount of stress on the Achilles tendon is the first step in treating tendinopathy. This can be achieved by modifying the amount of stress/load placed on the tendon. However, completely stopping any exercise/load should be avoided as it can cause atrophy and doesn’t fix the issue.
Manual therapy: Joint mobilisation can be used if joint restriction is present, and soft tissue techniques can be used to facilitate increased healing of the tissues as well as pain modulation.
Taping: Rigid taping can be used to decrease the strain on the Achilles tendon and/or alter foot posture in patients with Achilles tendinopathy.
Dry needling: Dry needling can be utilised in combination with exercise rehab.
Medication: Over the counter pain medication, may be an option is some cases but shouldn’t be the first line of treatment.
Achilles tendinopathy can be a painful and debilitating condition, but with proper treatment, it can be managed. It is important to seek medical attention as soon as possible if you are experiencing symptoms in order to start the recovery process. With the correct rehab, Achilles tendinopathy can be rehabilitated well and efficiently.
What if your back pain isn’t just from one bad movement — but from constantly living on the edge of your spine’s limits? This is
One of the most overlooked causes of persistent low back pain is how we move during everyday tasks. Simple activities like bending, sitting, getting out of a car, or
If you’ve been told your back pain is “non-specific” or has “no clear cause,” you’re not alone. Up to 85% of people with low back