The Importance Of Spare Capacity – Why Your Spine Needs A Safety Margin
What if your back pain isn’t just from one bad movement — but from constantly living on the edge of your spine’s limits? This is

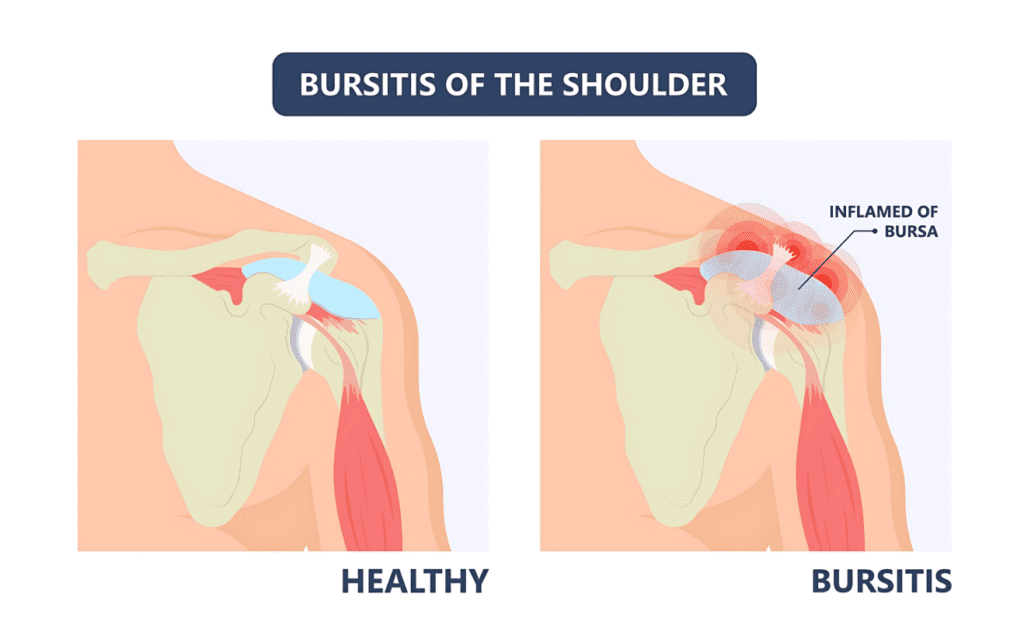
Bursitis is a condition that causes inflammation of the bursae, which are small fluid-filled sacs that cushion bones, tendons, and muscles near joints. It can lead to pain, swelling, and limited mobility. However, bursitis is most often a secondary issue—meaning that something else is causing irritation to the bursa, which then leads to inflammation. To truly treat bursitis effectively, the root cause must be identified and addressed rather than just managing inflammation.
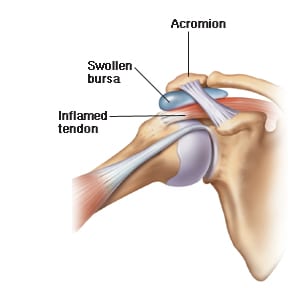
Bursae are found throughout the body, especially near major joints like the shoulder, elbow, hip, knee, and ankle. Each bursa is lined with a synovial membrane that secretes synovial fluid, reducing friction and allowing smooth movement between bones, tendons, and muscles.
Functions of the bursae include:
Bursitis itself is not the primary problem in most cases—it develops because of an underlying mechanical issue, repetitive strain, poor biomechanics, or another contributing factor. Simply treating the inflamed bursa without addressing what caused the irritation in the first place will often lead to recurrence.
Common underlying causes include:
Identifying and correcting the root issue is essential to resolving bursitis long-term.
Depending on which bursa is affected, bursitis can occur in different locations:

Since bursitis is usually secondary to another issue, some common contributing factors include:
Since bursitis is often a symptom of a bigger problem, treatment should go beyond short-term inflammation management. While initial care focuses on reducing pain and inflammation, long-term resolution requires identifying and correcting the underlying cause.
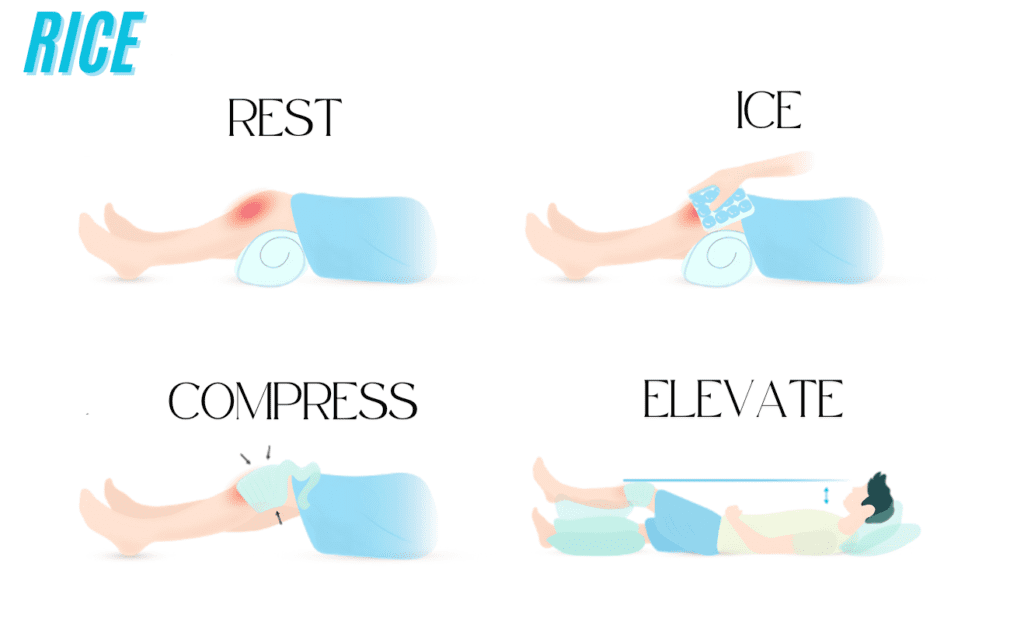
Initial Symptom Management:
Long-Term Treatment & Prevention:
To minimize the risk of bursitis returning, consider:
Bursitis is not just about inflammation—it’s a secondary condition caused by an underlying mechanical or functional issue. To fix bursitis for good, you need to find and correct the root cause, whether it’s a movement dysfunction, muscle imbalance, or poor biomechanics. Seeking treatment from a Soft Tissue Occupational Therapist can help address these issues and prevent recurrence.
What if your back pain isn’t just from one bad movement — but from constantly living on the edge of your spine’s limits? This is
One of the most overlooked causes of persistent low back pain is how we move during everyday tasks. Simple activities like bending, sitting, getting out of a car, or
If you’ve been told your back pain is “non-specific” or has “no clear cause,” you’re not alone. Up to 85% of people with low back