The Importance Of Spare Capacity – Why Your Spine Needs A Safety Margin
What if your back pain isn’t just from one bad movement — but from constantly living on the edge of your spine’s limits? This is

If you’ve been battling persistent low back pain without clear answers, shear instability could be the missing piece of your puzzle.
While disc bulges, muscle strains, and degenerative changes often receive the spotlight, shear instability — subtle, uncontrolled movement between spinal segments — is a major, yet frequently overlooked, driver of chronic pain, as described by renowned spine researcher Professor Stuart McGill.
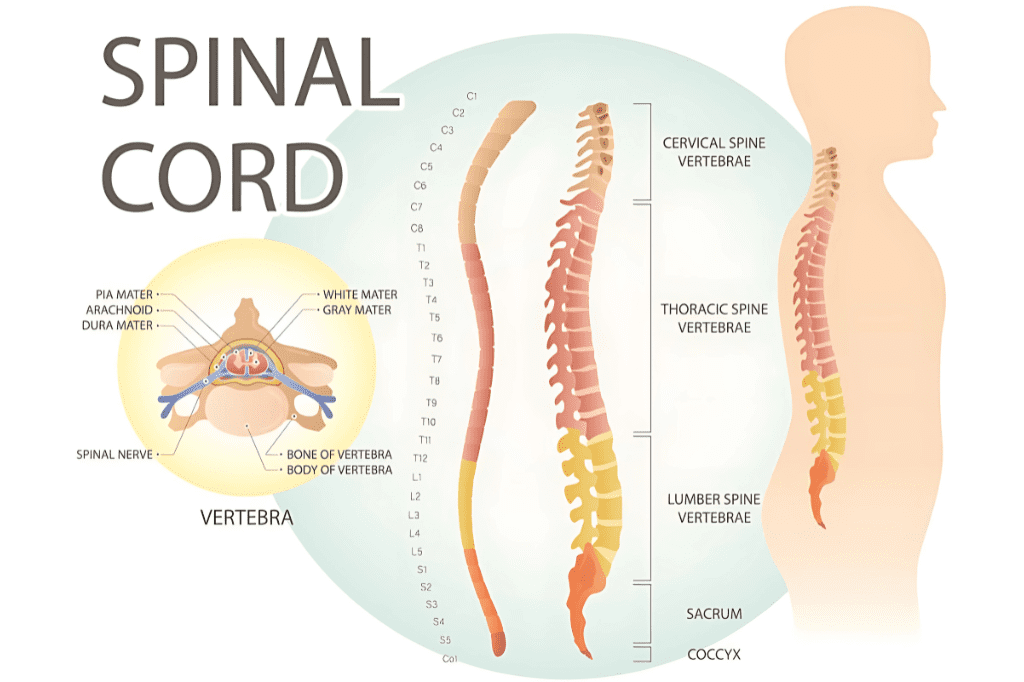
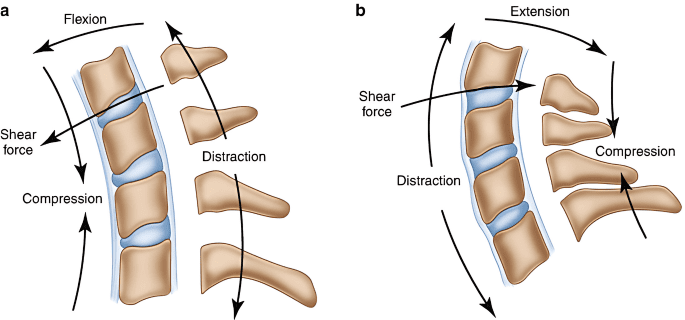
The spine is structurally designed to withstand heavy compressive forces. However, it is inherently vulnerable to shearing forces — sliding forces where one vertebra translates or shifts relative to another.
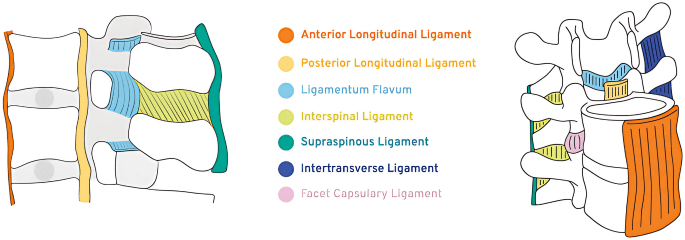
In a healthy, resilient spine, passive structures like ligaments, and active control mechanisms provided by spinal muscles, work together to resist shear. When these systems fail — whether through injury, deconditioning, or cumulative overload — the result is micro-movement at the segmental level. Over time, these small uncontrolled movements cause persistent irritation and sensitization of pain-generating tissues like discs, facet joints, and nerves.
This is shear instability: not a visible “tear” or “fracture,” but a hidden loss of mechanical integrity that keeps tissues irritated and pain lingering.
Recognizing shear instability requires a careful clinical eye, as it often presents subtly. Key indicators include:
If these symptoms sound familiar, shear instability could be an underlying factor.
Conventional rehabilitation frequently falls short because it does not target the underlying mechanical dysfunction. General stretching programs can inadvertently worsen instability, while random strengthening efforts might overload vulnerable structures.
McGill’s approach to rehabilitation emphasizes “spine-sparing” strategies and the creation of a “stiffness shield” — a protective mechanism built through precise movement correction and targeted muscle endurance training.
Successful management of shear instability follows a structured, evidence-informed path:
A structured, patient-specific approach is essential to break the cycle of recurrent pain and vulnerability.
If you suspect that shear instability may be driving your persistent back pain, the path forward lies not in endless passive treatments, but in an individualized mechanical assessment and a carefully designed rehabilitation program.
At Perth Injury & Pain CLinic, our team conducts comprehensive mechanical assessments to help identify contributing factors like shear instability. For complex or challenging cases, consultations with one of our McGill Method certified practitioners — the only practitioners in Western Australia holding this advanced certification — are available to guide you through a structured, evidence-based recovery plan.
Book your initial assessment today and start rebuilding the foundation for a pain-free, resilient spine!
What if your back pain isn’t just from one bad movement — but from constantly living on the edge of your spine’s limits? This is
One of the most overlooked causes of persistent low back pain is how we move during everyday tasks. Simple activities like bending, sitting, getting out of a car, or
If you’ve been told your back pain is “non-specific” or has “no clear cause,” you’re not alone. Up to 85% of people with low back