Frozen shoulder (adhesive capsulitis) is often described as a mysterious condition that simply “appears.” But it rarely occurs without an underlying reason. At Perth Injury & Pain Clinic, we help you understand the two critical factors that drive frozen shoulder: a Supply Issue (reduced healing capacity) and a Demand Issue (too much stress on the tissue).
Most people have a combination of both — and once these are identified, recovery becomes far more predictable.


In this episode of The Soft Tissue OT Podcast, we dive deeper into the real causes behind frozen shoulder, the supply vs demand framework, and what you can do to support long-term recovery.

Frozen shoulder, also known as adhesive capsulitis, occurs when the shoulder capsule becomes thickened, tight, and inflamed. Over time, this leads to reduced movement, stiffness, and significant pain — especially during certain ranges of motion.
Inside the capsule, fibroblastic activity increases, collagen fibres thicken, and adhesions begin to form. This creates the hallmark features of frozen shoulder: pain, loss of mobility, and resistance to stretching.
But here’s the key:
Frozen shoulder develops because something is affecting your shoulder’s ability to heal (Supply Issue), or something is overloading the tissues (Demand Issue). Most cases involve a mix of both.
Reduced Healing Capacity
(Click to find out more)
Your shoulder relies on a steady supply of nutrients, oxygen, circulation, and hormonal balance to repair normal tissue stress. When this “healing supply chain” is disrupted, even small irritations can snowball into larger inflammatory responses.
Common Supply Issues include:
Cardiovascular conditions
Poor circulation
Hormonal changes (common in perimenopause/menopause)
Diabetes or insulin resistance
Thyroid dysfunction
Autoimmune conditions
Chronic stress or poor sleep
Reduced metabolic health
Post-surgical shoulder trauma
When healing capacity drops, the capsule can become increasingly sensitive, inflamed, and fibrotic — leading to frozen shoulder.
Too Much Stress on the Tissue
(Click to find out more)
Even a healthy shoulder can struggle if the demands placed on it exceed its tolerance. Frozen shoulder often develops after a period of:
Increased overhead activity
Lifting heavier loads than usual
Repetitive shoulder strain
Poor mechanics or posture
Returning to activity too soon after injury
Micro-irritations that accumulate over weeks or months
When tissues are repeatedly overloaded, tiny injuries occur. If the demand stays high and recovery remains low, inflammation builds — eventually contributing to capsular thickening and stiffness.

A proper assessment does more than measure how far your shoulder can move. At Perth Injury & Pain Clinic, we look at:
Shoulder mechanics and capsule irritability
Strength and stability of surrounding muscles
Scapular coordination
Posture and movement patterns
Sleep, metabolic health, and general recovery factors
Signs of hormonal or circulatory contributors
Previous injuries or periods of immobilisation
Pain triggers vs pain relievers
This allows us to pinpoint the exact factors contributing to your frozen shoulder — and create a plan that restores both healing capacity and shoulder function.
Frozen shoulder recovery works best when treatment addresses both the stiffness in the shoulder and the factors influencing how well your body can heal. Rather than forcing movement or relying on a single technique, our approach focuses on restoring mobility, improving healing capacity, and rebuilding strength in a way that respects the sensitive shoulder capsule.
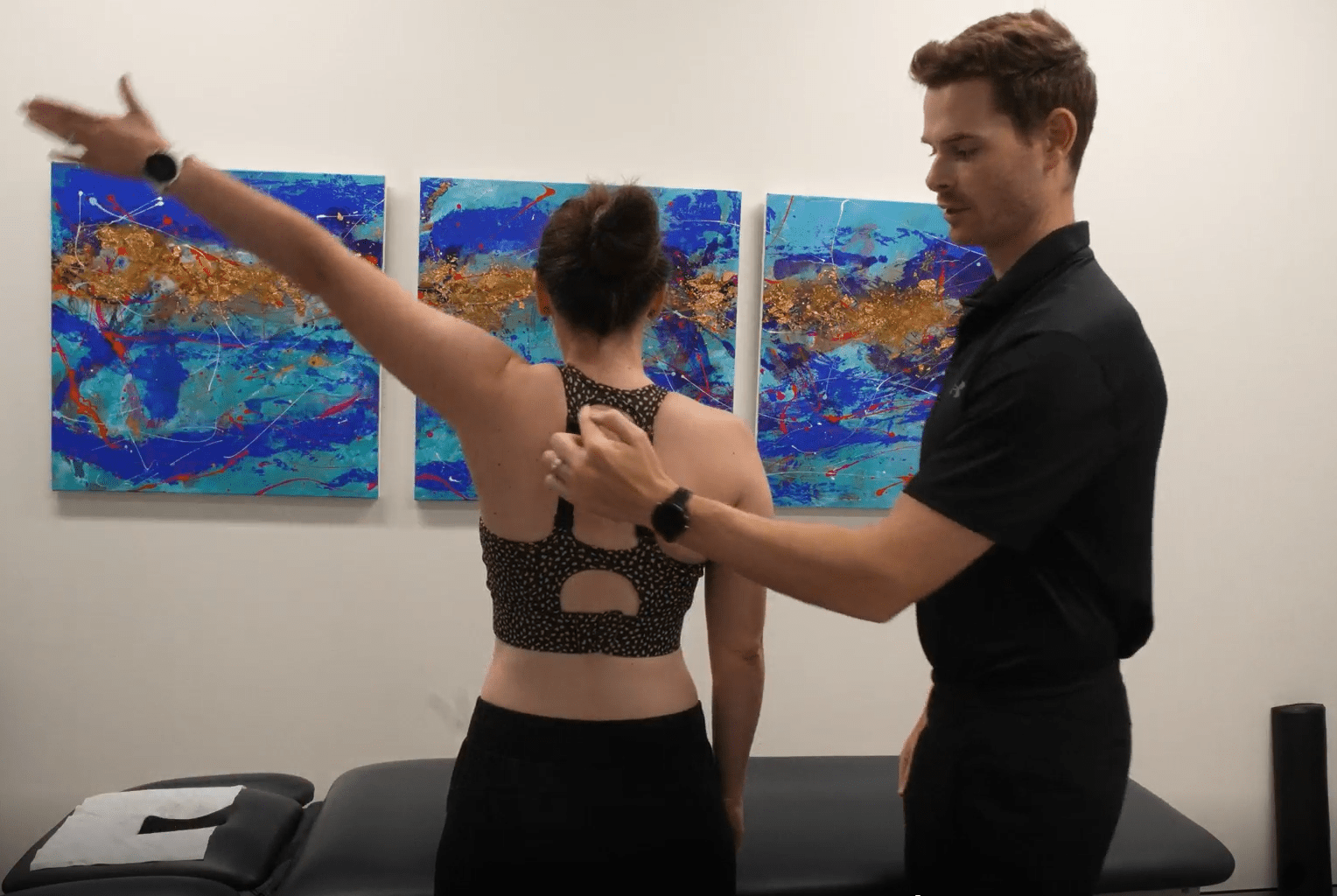
Frozen shoulder causes the shoulder capsule to become thickened and irritable, leading to restricted movement and pain. The goal at this stage is to gently improve shoulder mobility without further irritating the capsule. This is done through carefully selected movements that respect pain thresholds and adapt as your shoulder responds.

Frozen shoulder is strongly influenced by the body’s ability to heal. If circulation, hormonal balance, or metabolic health is compromised, recovery can be slower. Supporting healing capacity helps create an environment where the shoulder can settle and adapt more effectively.

As pain settles and movement improves, strengthening becomes essential. The aim is to support the shoulder joint so that everyday activities place less strain on the capsule. Strength is introduced progressively, with a focus on control, coordination, and confidence rather than heavy loading early on.
Frozen shoulder, medically known as adhesive capsulitis, is a condition where the shoulder capsule becomes inflamed, thickened, and stiff. Over time, this leads to pain and a significant loss of shoulder movement. The stiffness is not just muscular — it comes from changes within the joint capsule itself, including increased fibrotic tissue and reduced elasticity.
Frozen shoulder rarely develops without a reason. It is usually the result of a combination of two factors:
A supply issue, where the body’s ability to heal is reduced (for example due to hormonal changes, metabolic conditions, circulation issues, or systemic health factors), and
A demand issue, where the shoulder tissues are exposed to more load or stress than they can tolerate.
Most people experience a mix of both, which is why identifying the underlying contributors is critical for recovery.
Frozen shoulder can improve over time, but recovery is often slow and unpredictable without appropriate guidance. While some people eventually regain movement, stiffness and pain can persist for months or even years if the underlying supply and demand factors are not addressed. A structured approach can help support recovery and reduce unnecessary flare-ups.
The timeline varies significantly between individuals. Some people experience improvement within several months, while others take longer. Recovery depends on factors such as overall health, activity levels, metabolic or hormonal influences, and how the shoulder is managed during the painful and stiff phases. Addressing both healing capacity and tissue load can help guide a more efficient recovery.
Our approach focuses on identifying the true drivers behind your frozen shoulder. By understanding your individual supply and demand factors, we tailor a plan that supports healing capacity, restores movement safely, and rebuilds shoulder function over time — rather than simply treating symptoms.